From basic research to potentially practice-changing clinical trial results, last week’s AACR Annual Meeting 2025 showcased the exciting directions under investigation across the subfields of cancer research. Similarly, April’s Editors’ Picks from the AACR’s 10 peer-reviewed journals also highlighted research spanning the cancer research continuum, with fundamental insights into cancer metabolism and evolution, disparities in cancer incidence among Hispanic/Latino individuals with different heritage, and the clinical efficacy of new treatment approaches for leukemia and sarcoma, among other topics.
Read on for the abstracts of April’s Editors’ Picks, and follow the links for the full text of each article, freely available for a limited time.
Journal: Blood Cancer Discovery
Patients treated with chimeric antigen receptor T-cell (CAR-T) therapy are subject to profound immunosuppression. Dynamics of immune reconstitution (IR) and impacts of IR on outcomes following infusion across CAR-T products are not well understood. In this study, we profiled IR in 263 patients with relapsed/refractory large B-cell lymphoma receiving CAR-T therapy (axicabtagene ciloleucel 44.9%, lisocabtagene maraleucel 30.4%, and tisagenlecleucel 24.7%). Following infusion, patients remain persistently immunosuppressed, with 48.1% having CD4+ T-cell counts <200/µL and the median CD3-CD19+ B-cell counts remaining zero through 1 year after CAR-T therapy. IR differences exist by product, with the fastest CD4+ T-cell recovery seen for tisagenlecleucel, driven primarily by more rapid recovery of the CD4+CCR7−CD45RA− effector memory subset. NK cell, but not CD4+ T cell, recovery is significantly associated with favorable progression-free (HR, 0.65; 95% confidence interval, 0.48–0.88) and overall survival (HR, 0.64; 95% confidence interval, 0.44–0.92) and inversely correlated with inflammatory markers measured at the time of infusion.
Significance: This study reveals differences in IR patterns after CAR-T therapy in patients with large B-cell lymphoma, with early NK cell recovery emerging as a key predictor of survival. These findings provide potential future avenues of research for improving patient outcomes and tailoring post-therapy management strategies to mitigate relapse risk.
Journal: Cancer Discovery

In patients with non-small cell lung cancer (NSCLC), the relationship between tumor metabolism and clinical outcomes is unknown. Here, 13C-labeled nutrients were intraoperatively infused into more than 90 patients with surgically resectable pulmonary lesions, and metabolic properties of resected tumors were correlated with survival. In NSCLCs infused with 13C-glucose, high 13C enrichment in tricarboxylic acid (TCA) cycle intermediates conferred a HR of 3.8 for early death, typically with metastasis. To test whether these features reflect requirements for metastasis, we generated patient-derived xenografts that spontaneously metastasize to multiple organs. Treatment with an electron transport chain (ETC) inhibitor reduced glucose-derived TCA cycle labeling but did not suppress subcutaneous tumor growth. However, ETC blockade reduced the abundance of circulating cancer cells and suppressed xenograft metastatic burden in distant organs. Our data demonstrate that isotope labeling can identify metabolic properties associated with metastasis in patients and that blocking the ETC suppresses metastasis in mice.
Significance: Intraoperative 13C-glucose infusions in patients with NSCLC show that tumors with high labeling of TCA cycle intermediates progress rapidly, resulting in metastasis and early death. Blocking this pathway suppresses metastasis of human NSCLC cells in mice.
This article was featured on the cover of the April issue.
Journal: Cancer Epidemiology, Biomarkers & Prevention
Background: Few studies have examined how cancer incidence varies by the country of origin among US Hispanic/Latino adults. In this study, we describe the incidence rates (IR) of cancer overall and for screen-detectable, tobacco-related, and obesity-related cancers among 16,415 participants in the Hispanic Community Health Study/Study of Latinos, an ongoing population-based cohort study of Hispanic/Latino adults from diverse backgrounds.
Methods: Cohort participant records were linked to the state cancer registries in New York, Florida, California, and Illinois to ascertain cancer incidence from baseline (2008–2011) through 2021. We estimated weighted age-adjusted IRs and age- and sex-adjusted HRs.
Results: Over a mean follow-up of 10.7 (SD = 2.0) years, 715 incident invasive cancers were diagnosed including 118 female breast, 102 prostate, and 79 bronchus and lung cancers. The IR of all cancers combined was 26.2 [95% confidence interval (CI), 22.6–30.2] per 10,000 (10K) person-years (py). The IRs were lowest among persons of Mexican descent [IR, 19.0 (95% CI, 15.0–24.1) per 10K py] and highest for those of Puerto Rican [IR, 36.6 (95% CI, 28.4–47.0) per 10K py] descent. Compared with those of Mexican descent, those of Puerto Rican, Cuban, and Dominican descent had higher hazards of cancer incidence; the incidence of obesity-related (HR, 2.37; 95% CI, 1.43–3.95) and tobacco-related (HR, 3.00; 95% CI, 1.58–5.71) cancers was also the highest among Puerto Ricans.
Conclusions: Cancer IRs varied by Hispanic/Latino heritage and were masked when Hispanics/Latinos were aggregated into a single group.
Impact: Understanding disparities in cancer risk by Hispanic/Latino heritage may help tailor cancer prevention and control strategies.
Journal: Cancer Immunology Research
Different PD-L1 Assays Reveal Distinct Immunobiology and Clinical Outcomes in Urothelial Cancer
Testing for PD-L1 expression by IHC is used to predict immune checkpoint blockade (ICB) benefits but has performed inconsistently in urothelial cancer clinical trials. Different approaches are used for PD-L1 IHC. We analyzed paired PD-L1 IHC data on urothelial cancer samples using the SP142 and 22C3 assays from the phase III IMvigor130 trial and found discordant findings summarized by four phenotypes: PD-L1 positive by both assays, PD-L1 positive by the SP142 assay only, PD-L1 positive by the 22C3 assay only, and PD-L1 negative by both assays double negative. PD-L1 positive by both assays and PD-L1 positive by the SP142 assay only urothelial cancers were associated with more favorable ICB outcomes and increased dendritic cell (DC) infiltration. SP142 PD-L1 staining co-localized with DC-LAMP, a DC marker, whereas 22C3 staining was more diffuse. PD-L1 positive by the 22C3 assay only urothelial cancers, associated with worse outcomes, were enriched in tumor cell (TC)–dominant PD-L1 expression. Multiplex IHC in an independent ICB-treated cohort confirmed that TC-dominant PD-L1 expression was associated with shorter survival. Using different PD-L1 assays, we uncovered that SP142 may preferentially stain PD-L1–expressing DCs, key to orchestrating antitumor immunity, whereas TC-dominant PD-L1 expression, which underlies a subset of “PD-L1–positive” specimens, is associated with poor ICB outcomes.
A related commentary was published in the April issue.
Journal: Cancer Prevention Research

Diet affects cancer risk, and plant-derived polyphenols exhibit cancer-preventive properties. Walnuts are an exceptional source of polyphenolic ellagitannins, converted into urolithins by gut microflora. This clinical study examines the impact of urolithin metabolism on inflammatory markers in blood and colon polyp tissue. We evaluate the effects of walnut consumption on urinary urolithins, serum inflammatory markers, and immune cell markers in polyp tissues obtained from 39 subjects. Together with detailed food frequency data, we perform integrated computational analysis of metabolomic data combined with serum inflammatory markers and spatial imaging of polyp tissues using imaging mass cytometry. LC/MS-MS analyses of urine and fecal samples identify a widely divergent capacity to form nine urolithin metabolites in this patient population. Subjects with higher urolithin A formation exhibit lower levels of several key serologic inflammatory markers, including C-peptide, soluble form of intracellular adhesion molecule 1, sIL-6R, ghrelin, TRAIL, sVEGFR2, platelet-derived growth factor (PDGF), and MCP-2, alterations that are more pronounced in obese individuals for soluble form of intracellular adhesion molecule 1, epithelial neutrophil–activating peptide 78, leptin, glucagon-like peptide 1, and macrophage inflammatory protein 1δ. There is a significant increase in levels of peptide YY associated with urolithin A formation, whereas TNFα levels show an opposite trend, recapitulated in an in vitro system with ionomycin/phorbol 12-myristate 13-acetate–stimulated peripheral blood mononuclear cells (PBMC). Spatial imaging of colon polyp tissues shows altered cell cluster patterns, including a significant reduction of vimentin and CD163 expression associated with urolithin A. The ability to form urolithin A is linked to inflammation, warranting further studies to understand the role of urolithins in cancer prevention.
Prevention Relevance: We evaluate cancer-protective effects of walnuts via formation of microbe-derived urolithin A, substantiating their functional benefits on serum inflammatory markers and immunologic composition of polyps in normal/obese subjects. Our approach incorporates personalized nutrition within the context of colonic health, providing the rationale for dietary inclusion of walnut ellagitannins for cancer prevention.
This article was featured on the cover of the April issue.
Journal: Cancer Research (April 1 issue)
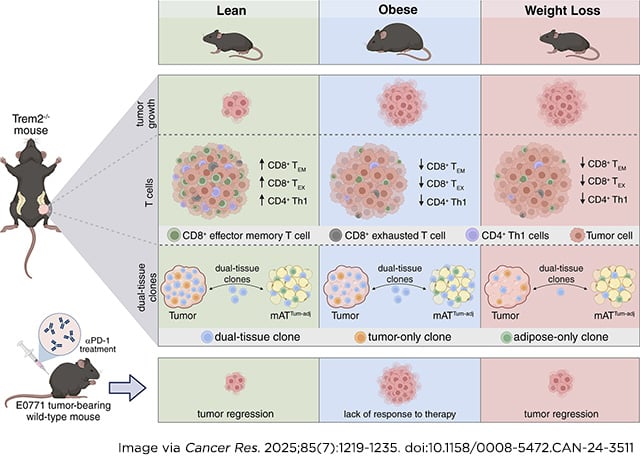
Obesity is an established risk factor for breast cancer development and poor prognosis. The adipose environment surrounding breast tumors, which is inflamed in obesity, has been implicated in tumor progression, and triggering receptor expressed on myeloid cells 2 (TREM2), a transmembrane receptor expressed on macrophages in adipose tissue and tumors, is an emerging therapeutic target for cancer. A better understanding of the mechanisms for the obesity–breast cancer association and the potential benefits of weight loss could help inform treatment strategies. In this study, we utilized lean, obese, and weight-loss mouse models to examine the impact of TREM2 deficiency on postmenopausal breast cancer depending on weight history conditions. Trem2 deficiency constrained tumor growth in lean, but not in obese or weight-loss, mice. Single-cell RNA sequencing, in conjunction with variable–diversity–joining sequencing, of tumor and tumor-adjacent mammary adipose tissue immune cells revealed differences in the immune landscapes across the different models. Tumors of lean TREM2-deficient mice exhibited a shift in clonal CD8+ T cells from an exhausted to an effector memory state, accompanied by increased clonality of CD4+ Th1 cells, that was not observed in any other diet-genotype group. Notably, identical T-cell clonotypes were identified in the tumor and tumor-adjacent mammary adipose tissue of the same mouse. Finally, anti–PD-1 therapy restricted tumor growth in lean and weight-loss, but not in obese, mice. These findings indicate that weight history could affect the efficacy of TREM2 inhibition in postmenopausal breast cancer. The reported immunologic interactions between tumors and the surrounding adipose tissue highlight significant differences under obese and weight-loss conditions.
Significance: Weight history impacts the immunological landscape of postmenopausal breast cancer and the efficacy of TREM2 modulation and anti–PD-1 therapy, which has implications for personalized medicine.
Journal: Cancer Research (April 15 issue)
Interactions between Ploidy and Resource Availability Shape Clonal Evolution in Glioblastoma

Glioblastoma (GBM) is the most aggressive form of primary brain tumor. The infiltrative nature of GBM makes complete surgical resection impossible. The selective forces that govern gliomagenesis are strong, shaping the composition of tumor cells during the initial progression to malignancy with late consequences for invasiveness and therapy response. Here, we developed a mathematical model that incorporates ploidy level and the nature of the brain tissue microenvironment to simulate the growth and invasion of GBM and used the model to make inferences about GBM initiation and response to the standard-of-care treatment. The spatial distribution of resource access in the brain was approximated through integration of in silico modeling, multiomics data, and image analysis of primary and recurrent GBM. The in silico results suggested that high-ploidy cells transition faster from oxidative phosphorylation to glycolysis than low-ploidy cells because they are more sensitive to hypoxia. Between surgeries, simulated tumors with different ploidy compositions progressed at different rates; however, whether higher ploidy predicted fast recurrence was a function of the brain microenvironment. Historical data supported the dependence on available resources in the brain, as shown by a significant correlation between the median oxygen levels in human tissues and the median ploidy of cancers that arise in the respective tissues. Taken together, these findings suggest that the availability of metabolic substrates in the brain drives different cell fate decisions for cells with different ploidy, thereby modulating both gliomagenesis and GBM recurrence.
Significance: Ploidy viewed in the context of the resources in the microenvironment has the potential to inform whether modulation of energetic availability can delay tumor progression and could help guide clinical decision making.
The article was featured on the cover of the April 15 issue.
Journal: Clinical Cancer Research (April 1 issue)
Purpose: We aimed to investigate the efficacy and safety of anlotinib as adjuvant targeted therapy for completely resected localized high-grade soft-tissue sarcomas (STS).
Patients and Methods: Patients with localized high-grade STS after complete resection were randomly assigned in a 1:1 ratio to receive either oral 12 mg anlotinib or placebo once daily on days 1 to 14 every 21 days as a cycle, with up to six cycles until disease relapse, unmanageable toxicity, or death. The efficacy and safety were analyzed. This trial was the first trial exploring adjuvant targeted therapy for STS (NCT03951571).
Results: Between June 2019 and November 2023, 88 patients were randomly assigned to receive anlotinib (n = 44) or placebo (n = 44). With a median follow-up of 30.95 months, the 1- and 2-year disease-free survival rates were 88% and 77% in the anlotinib group compared with 64% and 58% in the placebo group, respectively. Compared with patients treated with surgery alone, patients receiving adjuvant anlotinib combined with surgery had a reduced risk of disease recurrence [HR, 0.47; 95% confidence interval (CI), 0.22–1.00; P = 0.0445]. Based on the tumor histology, the reduced risk of disease recurrence with anlotinib versus placebo was observed in patients with myxofibrosarcoma (HR, 0.54; 95% CI, 0.17–1.65; P = 0.2698) and undifferentiated pleomorphic sarcoma (HR, 0.58; 95% CI, 0.12–2.87; P = 0.4971). Four patients discontinued anlotinib: two for proteinuria/hematuria (2/44, 5%) and two for poor healing of surgical wound (2/44, 5%).
Conclusions: Compared with surgery alone, adjuvant anlotinib following surgery reduces the incidence of disease relapse in localized high-grade STS, with acceptable toxicity.
Journal: Clinical Cancer Research (April 15 issue)
Purpose: To assess the efficacy and safety of an induction regimen composed of idarubicin, cytarabine, and cladribine (IAC) in patients with de novo acute myeloid leukemia (AML).
Patients and Methods: Adult patients with newly diagnosed AML were randomized to the IAC group (cladribine 5 mg/m2/day for 5 days, idarubicin 8 mg/m2/day for 3 days, and cytarabine 100 mg/m2/day for 7 days) and the IA group (idarubicin 12 mg/m2/day for 3 days and cytarabine 100 mg/m2/day for 7 days) at a 1:2 ratio. The primary endpoint was complete remission (CR) after induction. Secondary endpoints included 2-year overall survival (OS), disease-free survival, and cumulative incidence of relapse.
Results: A total of 618 adult patients with newly diagnosed AML were enrolled. The overall CR rate was 80.5% in the IAC group compared with 72.4% in the IA group (P = 0.029). The 2-year OS was 81.3% in the IAC group compared with 70.0% in the IA group (P = 0.011). Patients on the IAC regimen achieved a higher CR rate compared to those on the IA regimen, particularly in those with adverse risk (69.8% vs. 49.1%, P = 0.008), 2-year OS (80.1% vs. IA 58.1%, P = 0.014), and disease-free survival (78.8% vs. 51.3%, P = 0.009). In the subgroup of patients older than 45 years of age, the IAC regimen exerted better CR (77.1% vs. 62.6%, P = 0.033) and 2-year OS (74.7% vs. IA 55.0%, P = 0.019). There were no differences in chemotherapy-related toxicities between the groups.
Conclusions: Cladribine added to the IA regimen was safe and effective in de novo AML. Patients with adverse risk or those between 45 and 60 years of age might benefit significantly on both response and survival with the IAC regimen.
Journal: Molecular Cancer Research

Prostate cancer is mainly managed with androgen deprivation therapy (ADT), but this often leads to a dormant state and subsequent relapse as lethal castration-resistant prostate cancer (CRPC). Using our unique prostate cancer patient-derived xenograft dormancy models, we investigated this critical dormant phase and discovered a selective increase in B7-H4 expression during the dormancy period following mouse host castration. This finding is supported by observations in clinical specimens of patients with prostate cancer treated with ADT. Differential expression analyses revealed the enrichment of extracellular matrix (ECM)–cell interaction pathways in B7-H4–positive cells. Functional assays demonstrated a crucial role of B7-H4 in maintaining dormancy within the ECM niche. Specifically, B7-H4 expression in LNCaP cells reduced proliferation within the dormant ECM in vitro and significantly delayed relapse in castrated hosts in vivo. These results shed light on the dynamic regulation of B7-H4 during prostate cancer dormancy and underscore its potential as a therapeutic target for preventing CRPC relapse.
Implications: Our study identified membranous B7-H4 expression during ADT-induced dormancy, highlighting its potential as a therapeutic target for managing dormant prostate cancer and preventing fatal CRPC relapse.
This article was highlighted and featured on the cover of the April issue.
Journal: Molecular Cancer Therapeutics
Androgen receptor (AR) signaling is the principal driver of prostate cancer, and drugs that target this pathway (e.g., abiraterone and enzalutamide) are standard treatments for metastatic hormone-sensitive prostate cancer and metastatic castration-resistant prostate cancer. However, continual evolution during prostate cancer progression can result in AR alterations (e.g., mutation, amplification, and splicing) that can cause tumors to become resistant to these therapies. Bavdegalutamide (ARV-110) is a PROteolysis TArgeting Chimera (PROTAC) protein degrader that recruits the cereblon-containing E3 ubiquitin ligase to direct the polyubiquitination and subsequent proteasomal degradation of AR. Bavdegalutamide selectively degrades wild-type AR and most clinically relevant mutants with low nanomolar potency. The advantages of the degradation mechanism of action are demonstrated by the higher activity of bavdegalutamide relative to the AR antagonist enzalutamide in cell-based systems that assess effects on PSA synthesis, proliferation of prostate cancer cells, and induction of apoptosis. In an AR-expressing patient-derived xenograft mouse model, bavdegalutamide showed substantial AR degradation and greater tumor growth inhibition compared with enzalutamide. Bavdegalutamide also showed robust tumor growth inhibition in enzalutamide- and abiraterone-resistant prostate cancer animal models and enhanced activity in combination with abiraterone. These promising preclinical data supported the clinical development of bavdegalutamide as a potential treatment for patients with prostate cancer. Bavdegalutamide was the first PROTAC protein degrader to enter human clinical trials, specifically in patients with metastatic castration-resistant prostate cancer in a phase I/II study (NCT03888612).
This article was highlighted in the April issue.
Journal: Cancer Research Communications
The radiation sensitivity index (RSI) and 12-chemokine gene expression signature (12CK GES) are two gene expression signatures (GES) that were previously developed to predict tumor radiation sensitivity or identify the presence of tertiary lymphoid structures in tumors, respectively. To advance the use of these GESs into clinical trial evaluation, their assays must be assessed within the context of the Clinical Laboratory Improvement Amendments (CLIA) process. Using HG-U133Plus2.0 arrays, we first established CLIA laboratory proficiency. Then the accuracy (limit of detection and macrodissection impact), precision (variability by time and operator), sample type (surgery vs. biopsy), and concordance with a reference laboratory were evaluated. RSI and 12CK GES were reproducible (RSI: 0.01 mean difference, 12CK GES: 0.17 mean difference) and precise with respect to time and operator. Taken together, the reproducibility analysis of the scores indicated a median RSI difference of 0.06 (6.47% of range) across samples and a median 12CK GES difference of 0.92 (12.29% of range). Experiments indicated that the lower limit of input RNA is 5 ng. Reproducibility with a second CLIA laboratory demonstrated reliability with the median RSI score difference of 0.065 (6% of full range) and 12CK GES difference of 0.93 (12% of observed range). Overall, under CLIA, RSI and 12CK GES were demonstrated by the Moffitt Cancer Center Advanced Diagnostic Laboratory to be reproducible GESs for clinical usage.
Significance: The RSI and 12CK GES are two GESs that predict tumor radiation sensitivity or the presence of tertiary lymphoid structures in tumors, respectively. These GESs were assessed within the CLIA process for future clinical use. We established proficiency, reproducibility, and reliability characteristics for both signatures in a controlled setting, indicating these GESs are suitable for validation within future clinical trials.
The post Editors’ Picks, April 2025: Brain Cancer Evolution, New Treatment Approaches, and More appeared first on American Association for Cancer Research (AACR).