Strategies for overcoming hurdles for therapeutic translation, ways to target the cancer ecosystem, and advances in cancer vaccines were among the topics that had attendees talking during day four of the AACR Annual Meeting 2025. Read on for the takeaways from Tuesday, April 29 to get a flavor of today’s offerings and keep an eye on Cancer Research Catalyst, the official blog of the AACR, for more in-depth coverage of some of the cutting-edge science being presented at the AACR Annual Meeting 2025.
Plenary Session Examined the Cancer Ecosystem and Antitumor Immunity
“When we say cancer ecosystem, we are referring to the collection of mutationally perturbed cancer cells and the ostensibly normal stromal cells that coevolve with those cancer cells, and profoundly influence how they grow, spread, and respond to therapy,” said Mara H. Sherman, PhD, the chair of the “Targeting the Cancer Ecosystem” Plenary Session.
Yardena Samuels, PhD, first explored how different forms of tumor heterogeneity—at the genetic, transcriptomic, and proteomic levels—influence the repertoire of antigens that tumors present to the immune system and the power of subsequent antitumor immune responses. Samuels noted the need to quantify the degree of intratumoral heterogeneity in order to improve patient selection, especially with respect to immunotherapy. Overall, she proposed a process to extract valuable insights that could be leveraged clinically: first by mapping the recurrent clonal neoantigens within the “dark” proteome, then linking intratumoral heterogeneity to targetable antigens to counter potential immune evasion, and finally devising methods that account for this heterogeneity to reengineer the immunosuppressive tumor microenvironment.
Next, Matthew F. Krummel, PhD, explained how immune systems are partnerships that lead to dynamic emergent behavior, as he showed the audience a visual of a T cell and dendritic cell mingling their surfaces together to maximize the area for T cells to survey for presented antigens. This highlighted the emerging spectrum of “archetypes”—or collections of cells in linked states across tissue types—the immune system uses to meet a diverse spectrum of goals. Along with efforts to discover dominant immune archetypes reflected in tumor biology, Krummel shared his team’s strategy to develop “nudge” drugs to coax suboptimal immune archetypes within tumors toward more desirable states.
Though spatial heterogeneity, along with T-cell exclusion, is commonly seen in solid tumors, systematically measuring and interrogating it in human tumors and model systems has proven difficult, according to Kurt A. Schalper, MD, PhD. Noting that tumors with high baseline spatial heterogeneity were less responsive to immunotherapy, both alone and in combination with PARP inhibition, Schalper and his team analyzed spatial heterogeneity by integrating histology slides using computational algorithms to generate three-dimensional representations.
The final speaker, Mariam Jamal-Hanjani, MD, PhD, investigated how tumors spread and evolve dynamically throughout the body. “To truly understand the metastatic cascade, we need to take a holistic approach … that considers the cancer ecosystem,” she stressed.

To that end, Jamal-Hanjani has sought “to understand the process of lung cancer metastases from the perspective of the lung cancer and the environments in which it exists, but also the impact of metastases at the level of the whole body in the patient.” In this regard, she observed that tumors often have multiple clones with metastatic capacity, and that metastases-to-metastases seeding is common. Ultimately, this can lead to a divergence between the tumor microenvironments in primary and metastatic tumor sites, adding yet another layer of heterogeneity that must be confronted to improve care in the clinic.
Special Session Discussed Hurdles Facing Therapeutic Translation
In a Special Session organized by AACR President-Elect Keith T. Flaherty, MD, FAACR, and Timothy A. Yap, MBBS, PhD, presenters discussed the multitude of challenges facing therapeutic translation. These included biological hurdles such as acquired treatment resistance, tumor heterogeneity, and toxicities; logistical ones such as limited funding and rapid changes in technology; and philosophical ones such as conflicting perceptions about negative data and phase I clinical trial design.
“If I’ve learned one thing as an academic entrepreneur,” said Flaherty, “it’s that drug discovery and drug development are not linear.”
Presenters offered strategies to overcome these challenges, with many focusing on the importance of predictive biomarkers to not only identify patients likely to benefit from a therapeutic but also those who might develop resistance. Improving the technologies for tumor sampling to better capture the heterogeneity of each patient’s tumor was another approach recommended, as was utilizing digital twins or virtual clinical trials to model how a drug might impact a particular patient. One speaker stressed the value of learning from negative results, imploring attendees to “make every sample count,” and another explained the factors that influence whether or not investors choose to finance an experimental drug.
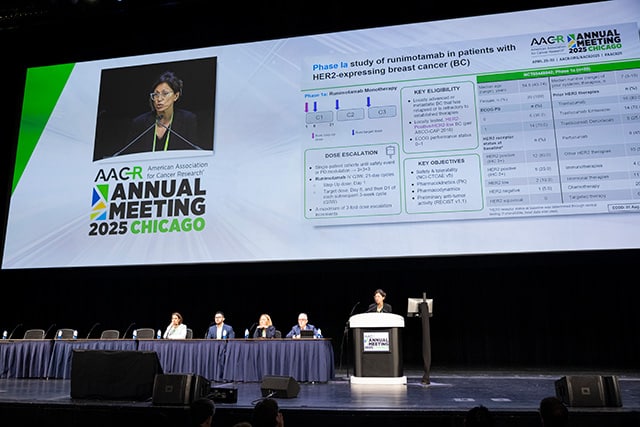
Clinical Trial Plenary Presented Updates on Antibody-based Therapies and CAR T Cells
Chaired by Jedd D. Wolchok, MD, PhD, FAACR, of Weill Cornell Medicine, and Crystal Mackall, MD, FAACR, of Stanford University, the “Biologics and T-cell Engagers” Clinical Trial Plenary session offered “an opportunity for us to think about how much change there has been in the use of immunotherapy agents to treat an ever-lengthening list of malignancies,” said Wolchok.
Juan C. Osario, MD, shared data on an Fc receptor-optimized antibody designed to stimulate the CD40 immune signaling pathway that led to complete tumor elimination in 38% of patients with non-muscle invasive bladder cancer that did not respond to Bacillus Calmette-Guérin vaccine. Shanu Modi, MD, presented results on the HER2 and CD3 bispecific antibody runimotamab in combination with trastuzumab in patients with HER2-positive breast cancer, showing that 30% of tumors responded. Invikafusp alfa, an antibody that targets T-cell receptor beta chain and the interleukin-2 receptor, led to a 61% disease control rate and a 52% tumor shrinkage rate across diverse types of antigen-rich, PD-L1 immunotherapy-resistant cancers, as highlighted by Ryan J. Sullivan, MD. Finally, Samer A. Srour, MD, revealed preliminary results from the first nine patients with advanced thyroid cancers who received the ICAM-1 CAR T-cell therapy AIC100, which led to one complete and one partial response.
Session on Cancer Vaccines Explored Recent Progress
Today’s Major Symposium on “Advances in Cancer Vaccines” continued the excitement from the Opening Plenary Session about recent progress in using vaccines to treat cancer.
During Sunday’s Opening Plenary, we learned that tumor-specific mutants called neoantigens are a “sweet spot” vaccine target, and, during today’s session, Stephen P. Schoenberger, PhD, suggested a new approach to identify candidate neoantigens—by isolating T cells from patient blood and determining which neoantigens they target.
Vinod Balachandran, MD, showed that a personalized mRNA neoantigen vaccine induced neoantigen-specific immune responses and delayed recurrence in patients with pancreatic cancer. And Darrell Irvine, PhD, discussed using albumin as a chaperone to guide peptide vaccines to lymph nodes, where adaptive immune responses are orchestrated.
Irvine, who was also the moderator of the session, noted that advances in vaccine technologies, experimental approaches, and clinical trial designs are “coming together and making for exciting progress happening currently in cancer vaccines.”
Poster Sessions Highlighted Research on Cancer Survivorship and Quality of Life
Among today’s Poster Sessions were two topics that are often top of mind for those who have to deal with the reality of having cancer: outcomes and survivorship.
During the session focused on “Health Disparities and Systemic Inequities: Lifestyle, Metabolism, and Disparities in Cancer Risk and Outcomes,” Adetunji Toriola, MD, PhD, MPH, presented an analysis of breast cancer mortality from the SEER Program 17 registry. Toriola and his colleagues found that even though breast cancer incidence rates in women ages 20 to 49 years have been increasing over the past 20 years, the incidence-based mortality rate of these patients has declined significantly from 9.70 per 100,000 women in 2010 to 1.47/100,000 in 2020.
A decline was found across all racial/ethnic groups and molecular subtypes, including luminal A, luminal B, HER2-enriched, and triple-negative breast cancer, with some variance in the level of decline but most of the pronounced differences were observed after 2016.
“The improvements in mortality likely reflect advancements in treatment options, greater uptake of precision medicine, and expanded access to care and screening in women aged 40-49,” Toriola explained. More specifically, he pointed to the broader adoption of CDK4/6 inhibitors and optimization of endocrine therapy, which began receiving FDA approval and clinical adoption between 2015 and 2016.
In the Poster Session on “Survivorship Research,” Simo Du, MD, MHS, of NYC Health + Hospitals/Jacobi and Montefiore Medical Center/Albert Einstein College of Medicine, examined the impact of cancer-related fatigue and depression on cancer survivors’ quality of life.
“During my residency, I saw a lot of cancer patients both in the clinic and inpatient settings, and cancer-related fatigue was one of the most frequent complaints they brought up,” Du said. “It impacts not just their daily activities but also their overall quality of life and mental health, making tasks like climbing stairs, doing groceries, or laundry overwhelming.”
In a retrospective study of data from the National Health and Nutrition Examination Survey (NHANES), Du and her colleagues found that cancer survivors who are experiencing cancer-related fatigue and depression are twice as likely to reduce their participation in recreational activities. Further, female cancer survivors are about 1.5 times more likely to experience cancer-related fatigue compared to male cancer survivors.
“Our findings highlight the importance of providing special attention and tailored interventions such as exercise programs, support groups, and mind-body behavioral techniques for vulnerable groups to help effectively manage fatigue and improve participation in recreational activities as they are an essential aspect of quality of life,” Du explained.
Dogs!
But the posters weren’t the only things driving excitement in the Exhibit Hall today. A handful of therapy dogs were also present, eagerly waiting for attendees to take a “paws” from science and enjoy some canine companionship.

Using Liquid and Tissue Biopsies Together to Identify Tailored Therapies for Patients
In a Minisymposium on “Targeted Therapies and Combinations,” one of the presenters touched on the potential value of optimizing the selection of tailored therapies for patients through the use of both tissue and liquid biopsy. In the phase II, multicenter ROME trial, next-generation sequencing was performed on tissue and blood samples from 1,794 adult patients between November 2020 and August 2023 and a molecular tumor board assessed the results to determine whether patients had a genomic alteration that could be targeted with therapy. Results were considered concordant if the same significant alterations were detected in both biopsy types, while discordance indicated detection in only one.

Of the 400 patients the board identified with an actionable alternation, tissue and liquid biopsies identified the same alteration in 49.2% of cases (197 patients), an alteration was exclusively detected via tissue biopsy in 34.7% of cases (139 patients) and exclusively in liquid biopsies in 16% (64 patients). In each arm, patients were randomly assigned to receive either tailored therapy or standard of care as chosen by the clinician presenting the case. Progression-free survival was longest in the tissue and liquid biopsy group (4.93 months) followed by the tissue-only group (3.06 months) and liquid-only group (2.07 months). Overall survival was also highest in the tissue and liquid biopsy group (11.05 months), followed by the tissue-only group (9.93 months), and the liquid-only group (4.05 months).
“The superior outcomes observed in patients with concordant biopsy findings highlight the potential of combined molecular profiling approaches to optimize patient selection for tailored therapies,” Paolo Marchetti, MD, of the Istituto Dermopatico dell’Immacolata (IDI-IRCCS), said in a press release announcing the results. “The concordance may be related to the tumor expressing the same genomic alteration in different metastatic sites. Expanding the analyses to account for more factors, such as disease subtype, metastatic sites, and biopsy location could help define a new, more effective diagnostic pathway.”
Probing the Origins of Childhood Cancer
While most cancers develop as a result of mutations that accumulate over the course of a lifetime, childhood cancers occur much earlier, before such damage has occurred. Today, in the Major Symposium “Developmental Origins of Childhood Cancer,” researchers converged to discuss how aberrations in development can cause pediatric malignancies.
“My ultimate goal is to use this symposium to reinvigorate discussion of the therapeutic vulnerabilities and the potential therapeutic opportunities to target developmental pathways and processes in childhood cancer,” said Corinne M. Linardic, MD, PhD, from Duke School of Medicine, who chaired the session.
Linardic reviewed the developmental underpinnings of rhabdomyosarcoma and showed how comparative proximity labeling and in-depth studies of oncogenic fusions could reveal potential new drug targets. Tim Coorens, PhD, from the Broad Institute of MIT and Harvard showed how lineage tracing can uncover the sequence of genetic events that lead to a particular cancer. Finally, Philip J. Lupo, MD, MPH, explored the relationship between birth defects and the development of childhood cancer and discussed how studying the genetic basis of one could lead to valuable insights about the other and vice versa.
Final Award Lectures Took Place
Attendees had the chance to hear from five more scientific honorees today as they delivered the last five award lectures of this year’s Annual Meeting.
Peter Westcott, PhD, spoke on “Deconstructing benign-to-malignant transition in the colon.” Westcott received the 2024 Gertrude B. Elion Cancer Research Award to support research aimed at understanding the earliest events in colorectal cancer development. Today’s lecture summarized some of the progress he has made from this research funding.

Loїc Le Marchand, MD, PhD, MPH, recipient of the AACR-American Cancer Society Award for Research Excellence in Cancer Epidemiology and Prevention, spoke on “Elucidating cancer etiology through multi-ethnic studies.” Le Marchand was recognized for elucidating racial and ethnic disparities in lung cancer risk and demonstrating the impact of visceral adiposity on cancer susceptibility.
Crystal L. Mackall, MD, FAACR, received the AACR-Cancer Research Institute Lloyd J. Old Award in Cancer Immunology in honor of her contributions to cancer immunotherapy, including enhancing CAR T-cell therapies, defining resistance mechanisms, advancing consensus treatment algorithms, and leading groundbreaking clinical trials. Her award lecture examined “CAR T cells for cancer.”
Louis M. Staudt, MD, PhD, FAACR, recipient of the AACR Award for Outstanding Achievement in Blood Cancer Research, discussed “Curing aggressive lymphomas using multi-drug combinations targeting oncogenic survival pathways.” Staudt received this award in recognition of his pioneering contributions to the molecular classification of diffuse large B-cell lymphoma.
Shelley L. Berger, PhD, FAACR, delivered the AACR-Women in Cancer Research Charlotte Friend Lectureship, which she was awarded in honor of her fundamental discoveries in cancer epigenetics, including how histone modifications and transcription factors regulate cancer, aging, and T-cell function. Her lecture was titled “Epigenetic pathways as targets in human cancer.”
Visit the virtual platform to view any of the scientific sessions or e-posters through October 2025. For more coverage of the meeting, go to AACR Annual Meeting News, check out the takeaways from each day, and subscribe to Cancer Research Catalyst.
The post Daily Takeaways From the AACR Annual Meeting 2025: Tuesday, April 29 appeared first on American Association for Cancer Research (AACR).