On the final day of the AACR Annual Meeting 2025, experts discussed opportunities in predictive oncology in a Plenary Session, and three thought leaders took a comprehensive look at the biggest discoveries across the cancer continuum presented during the conference. Read on for our takeaways from Wednesday, April 30 at the AACR Annual Meeting 2025. Continue to visit Cancer Research Catalyst or subscribe for email alerts, so you don’t miss our additional coverage of the meeting with deeper dives into the cutting-edge science that was presented.
Crafting Crystal Balls for Cancer
“Understanding one patient at a time … is the cornerstone of our strategy to improve cancer outcomes,” said David W. Craig, PhD, the chair of the “Opportunities in Predictive Oncology” Plenary Session.
“Predicting responses to treatment at the individual level, such as with immunotherapy, remains a critical challenge,” according to Craig, but cutting-edge multiomic and multiscale technologies are providing “new opportunities for decoding and understanding tumor behavior … and how to improve outcomes.”
“How is it possible that with an almost infinite number of mutational patterns, you end up having cancer cell states that are rather finite and limited in terms of their characteristics?” pondered Andrea Califano, Dr, FAACR, who shared novel concept of an “oncotecture” within each cell that keeps a pulse on and integrates all of the information regarding mutations and signaling activity to maintain homeostatic stability. Observing that most mutations appear more probabilistic than deterministic in dictating tumor cell state, Califano likened techniques confronting this complexity to “quantum” cancer therapy.
Christina Curtis, PhD, MSc, discussed efforts to create “digital twins” that replicate the dynamic behavior of life—at the molecular, cellular, and tissue levels, all of which are crucial in cancer. Demonstrating the ability to effectively incorporate and analyze information from these varied sources, Curtis shared her hope that this will be a first step toward models that allow for more anticipatory action by clinicians. “The tools are here to make the measurements. We have to pursue rich data capture … throughout the disease course and even before the onset of overt malignancy,” she stressed.

“Is secondary resistance the same entity that happens later, or is it something different?” asked Marleen Kok, MD, PhD, who shared insights into what differentiates long-term from short-term responders in immunotherapy-treated patients with triple-negative breast cancer. Particularly important for durable benefit were spikes in both tumor-targeting T cells and immune checkpoint expression after patients started immunotherapy, even more so than T cell numbers prior to treatment.
Regarding the potential for artificial intelligence to improve decision-making in the clinic, Trey Ideker, PhD, emphasized that “we need to have trust, transparency, and a full understanding of the rationale.” To that end, he showcased deep-learning systems embedded with structural tumor cell maps that shed light on novel, highly penetrant drug-mutation interactions involving members of the PARP family of DNA repair molecules.
Optimizing Lung Cancer Screening
The last few sessions reminded attendees that, although the meeting is ending, there’s plenty of work still to be done. Case in point: refining guidelines for lung cancer screening.
“We want to screen more people for lung cancer and catch it early, but the key problem we don’t understand is who is at risk for this disease,” said Lecia V. Sequist, MD, MPH. Sequist chaired the session, “Lung Cancer Screening: Promises and Pitfalls” as part of the Advances in Early Detection and Interception series.
In the session, sponsored by the Margaret Foti Foundation, researchers reviewed the current state of lung cancer screening in the United States and explained how far the field must go to reach optimal implementation. They also discussed how technologies like artificial intelligence and liquid biopsy may help streamline lung cancer screening and improve precision.
Addressing Care Gaps in Indigenous Populations
Another session, “Cancer and Indigenous Populations: From Risk Factors to Cancer Care Delivery to Policy,” called attention to the need to better address the gaps in the care of Indigenous populations. There are an estimated 8.8 million individuals in the United States who identify as American Indian/Alaska Native alone or in combination with one or more other races.
“When we are talking about Indigenous nations, we’re not just talking one homogenous whole, we’re talking about 574 federally recognized Tribal Nations that doesn’t include the over 400 unrecognized Tribal Nations and urban Indigenous peoples,” explained Krystal Tsosie, PhD, MPH. “Because we have distinct cultural histories and geographies, we also have distinct genetic histories.”
Tsosie said that Indigenous people make up fewer than 1% of the participants in genome-wide association studies. However, she emphasized this is not necessarily due to a lack of engagement or awareness around these studies and how they could lead to advances in precision medicine, but more so a lack of trust over whether the data that participants contribute will ultimately be used to benefit Indigenous peoples. To address this, Tsosie helped form the Native BioData Consortium (NBDC), a biorepository that allows tribal members to have more ownership over their data and control over which studies the data can be used in.

“When you have a server on tribal lands that operates under tribal laws and jurisdiction … you have an opportunity to build a data infrastructure that doesn’t replicate the same problems that we see in non-tribal settings,” Tsosie said.
Partnering directly with tribal populations was also a key point made by the other two speakers—Dorothy A. Rhoades, MD, MPH, and Rodney Haring, PhD, MSW—who addressed how cancer centers can better serve Indigenous peoples. For example, at the Stephenson Cancer Center, Rhoades is working on a pilot program to improve care coordination among the patient, the oncology team, a Native American patient navigator, and Indian Health Service or an Urban Indian Organization. While Haring showed a map examining existing cancer centers near tribal lands and pointed to a lack of NCI-designated cancer centers in both the Great Plains and Alaska, he also made it clear that all existing cancer centers are likely to serve some Indigenous individuals.
“If your cancer center or university or practice hasn’t worked with the tribes in your region … that really needs to change,” Haring said.
Final Session Showcased the Main Takeaways From AACR Annual Meeting 2025

The meeting concluded with the “AACR Annual Meeting 2025 Highlights: Vision for the Future” Plenary Session, which spotlighted the themes, findings, and impact of the great science reported over the past six days. Three speakers, each representing a different branch of cancer research, examined the meeting’s highlights across the continuum of cancer research.
Cory Abate-Shen, PhD, covered basic cancer science and translational research, identifying advances in chemistry, genomics and epigenomics, tumor cell states and heterogeneity, and understanding the tumor ecosystem as some of the key themes that emerged from the meeting. She noted that fundamental insights within each of these categories are advancing the ability to overcome treatment resistance, develop innovative therapeutic strategies, and go after new targets.
In the fields of cancer prevention, early detection, population sciences, and disparities, Scarlett Lin Gomez, PhD, MPH, pointed to presentations on early-onset cancer, emerging risk factors, community-centered communication and interventions, and screening disparities as highlights that not only showed the progress that has been made but also demonstrated the need for more research and larger and more inclusive datasets.
Finally, Jayesh Desai, MBBS, cochair of the Annual Meeting Clinical Trials Committee, summarized key findings from the multitude of clinical trial data reported during the meeting. He noted that immune checkpoint inhibitors helped some patients avoid surgery and improved outcomes for head and neck cancer; ctDNA flexed its muscle in guiding treatment and monitoring responses and recurrence; new therapeutic targets, including the Werner helicase, showed promise; and innovative approaches advanced the use of T-cell therapies for solid tumors.
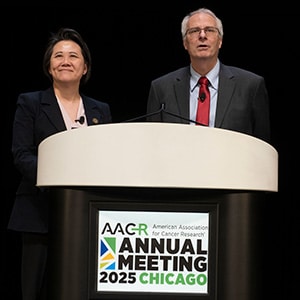
“I really enjoyed and learned a lot this week at the meeting about the continuum of cancer science and medicine,” said Matthew G. Vander Heiden, MD, PhD, who, alongside AACR President Lillian L. Siu, MD, FAACR, served as session moderator and Annual Meeting program chair. “The science was absolutely fantastic.”
That’s a Wrap—See You Next Year!
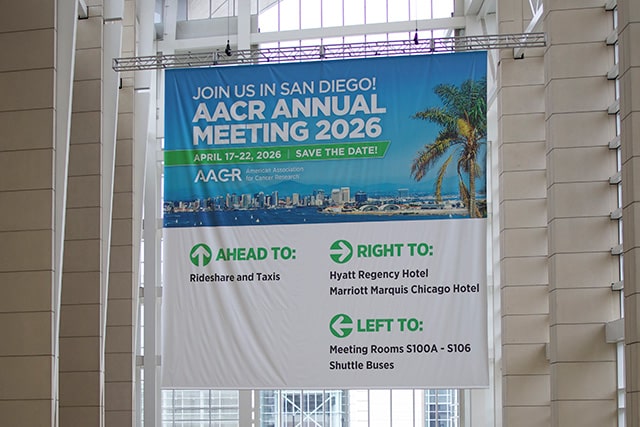
Visit the virtual platform to view any of the scientific sessions or e-posters through October 2025. For more coverage of the meeting, go to AACR Annual Meeting News and check out the takeaways from each day.
The post Daily Takeaways From the AACR Annual Meeting 2025: Wednesday, April 30 appeared first on American Association for Cancer Research (AACR).